Special histology
Central and peripheral nervous system
Cardiovascular system
Blood and the bone marrow
The immune system and lymphoid organs
The digestive system
Organs associated with the digestive system
The respiratory system
The skin and its derivates
The urinary system
The endocrine system
The male reproductive system
The female reproductive system
Organs of special sense
The central and peripheral nervous system
The central nervous system
The specimen is the spinal cord, medulla spinalis (HE). On a cross-section of the spinal cord, the central canal can be seen. The central canal is lined by a single layer of cubic ependymal cells - specialized glial cells. Surrounding this canal an area of gray matter can be seen, while the white matter is located peripherally. In the gray matter, there are perikaryons of multipolar nerve cells, with a clearly visible nucleus and basophilic cytoplasm filled with Nissl bodies or tigroid (clusters of granular endoplasmic reticulum). Around the perikaryon is the neuropil, which consists of a network of nerve fibers, glial cells (microglia, astrocytes, oligodendrocytes) and blood capillaries. In the white matter area, we find myelinated nerve fibers, some glial cells and capillaries. Since myelin is dissolved during the preparation of the preparation, the fibers are surrounded by white (empty) space.
The specimen is the spinal cord, medulla spinalis (silver impregnation). On a cross-section of the spinal cord, the central canal of the spinal cord can be seen, surrounded by an area of gray matter, while the white matter is located peripherally. In the gray matter, there are darkly stained perikaryons of multipolar nerve cells with a light-colored nuclear area. Around the perikaryon is the neuropil, which consists of a network of black-stained nerve fibers, the nuclei of glial cells (microglia, astrocytes, oligodendrocytes) and blood capillaries. In the white matter area, we find myelinated nerve fibers, some glial cells and capillaries.
The specimen is a cross-section through the small brain or cerebellum (HE). At low magnification, the folds (sulci and gyri) of the cerebellum can be seen, as well as the arrangement of gray and white matter within them. These resemble a branched tree crown and is therefore also called the tree of life or arbor vitae. The surface of the cerebellum is covered with a soft meningeal membrane - the pia mater. At its surface is the cortex or gray matter, made up of three well-defined layers (going from the surface inwards): the molecular layer (stratum moleculare) the Purkinje cell layer (stratum gangliosum) and the granular layer (stratum granulosum). In the molecular layer, the nuclei of basket and stellate cells and the neuropil - a dense network of fibers of the cells of the molecular layer as well as the fibers of the cells located in the granular layer and the dendrites of the Purkinje cells are visible. The stratum gangliosum is made up of one layer of large Purkinje cells whose dendrites branch in the molecular layer, and the axon goes into the granular layer. The granular layer is made up of numerous granular and Golgi cells as well as nerve fibers. In some places between the perikaryons of the cells there are areas without cells called parenchymatous islands or glomerula cerebellaria. They represent the sites of synapses of the cells of the cerebellar cortex with fibers coming from the white matter. Throughout the gray matter we find numerous blood capillaries. In the white matter area we find myelinated nerve fibers, some glial cells and capillaries. As the myelin is dissolved during the preparation of the specimen, the fibers are surrounded by white space..
The preparation is a cross-section through the small brain or cerebellum (silver impregnation). At low magnification, the furrows and convolutions, sulci and gyri of the cerebellum can be seen, as well as a certain arrangement of gray and white matter within them, which resembles a branched tree crown and is called the tree of life or arbor vitae. The surface of the cerebellum is covered with a soft meningeal membrane - the pia mater. O At its surface is the cortex or gray matter, made up of three well-defined layers (going from the surface inwards): the molecular layer (stratum moleculare) the Purkinje cell layer (stratum gangliosum) and the granular layer (stratum granulosum). In the molecular layer, the nuclei of basket and stellate cells and the neuropil - a dense network of fibers of the molecular layer cells as well as the fibers of the cells located in the granular layer and the dendrites of the Purkinje cells are visible. The stratum gangliosum consists of one layer of large Purkinje cells whose dendrites branch in the molecular layer and the axon goes into the granular layer. At high magnification, you can see the "baskets" surrounding the Purkinje cells. These are collateral shoots of the axons of the basket cells that form networks around the perikaryon of the Purkinje cells. The fibers are easily visible because they are colored black with this staining method. The granular layer is made up of numerous granular and Golgi cells as well as nerve fibers. Numerous blood capillaries are found throughout the gray matter. Myelinated nerve fibers are found in the white matter, which is stained dark brown to black with this method, so that the entire white matter area appears dark.
The preparation is a part of the large brain, the cerebrum (HE). The greater part of the preparation is made up of the cerebral cortex, made up of gray matter with numerous perikaryons of nerve cells. There are pyramidal and non-pyramidal neurons (granular, stellate, horizontal cells) arranged in six layers that cannot be differentiated well on the preparation. These are, from the surface to the inside: lamina molecularis, lamina granularis externa, lamina pyramidalis externa, lamina granularis interna, lamina pyramidalis interna and lamina multiformis. At high magnification, the triangular appearance of pyramidal neurons can be seen, from the base of which the axon emerges, and from the sides the dendrites. On part of the preparation, white matter or medulla made up of myelinated nerve fibers can be seen. Since myelin is dissolved during preparation of the preparation, the fibers are surrounded by white (empty) space. Throughout the specimen, we find a large number of blood capillaries.
The cardiovascular system
The heart
The specimen is the inner part of the heart wall, the endocardium (HE). The endocardium consists of the endothelium with its supporting connective tissue, a middle myoelastic layer of smooth muscle cells and elastic connective tissue and a subendocardial layer of connective tissue. The endocardium is connected to the heart muscle, the myocardium, by the subendocardial connective tissue in which large, bright Purkinje cells belonging to the cardiac conduction musculature can be seen. The myocardium is the layer of the heart made up of the working musculature of the heart (cross-sectioned cardiac muscle fibers). In this specimen, a purkinje fiber can be seen to deeply enter the myocardium. The myocardium is highly nutrient and oxygen-intensive and the endomysium therefore contains a large number of blood capillaries.
The specimen is the outer part of the heart wall, the epicardium (HE). The epicardium covers the outer surface of the heart and forms the visceral layer of the pericardium. It is covered by mesothelium, under which connective tissue with numerous blood vessels, nerves and ganglia can be seen. Under the epicardium is adipose tissue, the so-called subepicardial fat tissue. The connective tissue enters the middle, muscular layer of the heart, the myocardium, alongside the larger blood vessels.
Blood vessels
The specimen is a cross-section of an artery, vein and (small) nerve (HE). The wall of an artery is made up of 1. the tunica intima: a layer of endothelium, a subendothelial layer of loose connective tissue of the lamina propria and a wavy, red-stained elastic membrane (membrana elastica interna; difficulat to discern on this specimen, but it can be clearly seen in Blood vessel II). 2. tunica media; a collection of thick bundles of smooth muscle cells. 3. tunica externa/adventicia; a layer of loose connective tissue via which the artery is connected with its surrounding tissues. In addition, a large vein can be seen. Its wall is made up of the same layers as the arteries. However, veins do not have the thick elastic layer in the tunica intima. Also, typically the tunica media is much thinner, whereas the adventicia is thicker. Veins also usually have a larger lumen. Vains also have valves to prevent blood from flowing back, but this cannot be seen on this specimen. A small nerve surrounded by connective tissue is also visible in cross-section on the preparation.
The specimen is a cross-section of an artery, vein, and nerve (HE). This slide shows similar histological structures as the previous one, but with a much larger nerve, allowing the distinction between the perineurium surrounding nerve bundles and the epineurium surrounding the entire nerve. At the top of the specimen, in the vein bordering the nerve, we can see a valve. Finally, we can clearly see the thick meandering elastic layer in the tunica intima of the artery.
The specimen is a cross-section of an elastic artery (orcein). The wall of the artery is made up of the tunica intima: a layer of endothelium, loose connective tissue of the lamina propria, and a wavy, darker brown colored elastic membrane (membrana elastica interna); tunica media: thick bundles of weakly stained smooth muscle cells separated from the next layer by a dark, wavy membrane (membrana elastica externa). Elastic arteries are characterized by a large number of elastic fibers, which arise from smooth muscle cells in this layer; tunica externa: a layer of loose connective tissue with which the artery has grown to the environment. Small veins can also be seen at the bottom of the specimen. Clearly, the tunica intima of these structures contain much less elastic fibers.
Blood and the bone marrow
Blood
The specimen is a blood smear (May-Grunwald-Giemsa). In addition to a large number of red blood cells - erythrocytes, white blood cells - leukocytes can be seen on the preparation, which can be segregated in granulocytes (neutrophils, basophils, eosinophils) and agranulocytes (monocytes, lymphocytes). Individual clusters of blood platelets - thrombocytes can also be seen on the preparation as small purple spots. Erythrocytes are biconcave discs without a nucleus. Neutrophils are cells with a segmented nucleus of which the granules do not stain. Therefore, their cytoplasm is clear or light basophilic. Basophils are rare cells with a segmented nucleus, eosinophilic cytoplasm, and blue-stained granules. Eosinophils are rare cells with a segmented nucleus, eosinophilic cytoplasm, and red-stained granules. Monocytes are large cells with a kidney-shaped nucleus and basophilic cytoplasm. Lymphocytes are small cells with a large round nucleus surrounded by a small rim of basophilic cytoplasm.
The bone marrow
The specimen is red bone marrow, medulla ossium rubra (decalcified, HE). In the specimen, red bone marrow can be seen between the pink-stained bone beds. The marrow is made of stroma (reticular cells and fibers), which in the preparation is covered with hematopoietic threads from different developmental stages of erythrocytes and leukocytes. At higher magnification, large birght pink multinuclear cells can be seen. These are megakaryocytes, which do not enter the bloodstream, but release platelets into the sinusoids. A greater number of sinusoidal capillaries and adipocytes can be seen in the specimen.
The immune system and the lymphoid organs
Primary lymphoid organs
The specimen is red bone marrow, medulla ossium rubra (decalcified, HE). In the specimen, red bone marrow can be seen between the pink-stained bone beds. The marrow is made of stroma (reticular cells and fibers), which in the preparation is covered with hematopoietic threads from different developmental stages of erythrocytes and leukocytes. At higher magnification, large birght pink multinuclear cells can be seen. These are megakaryocytes, which do not enter the bloodstream, but release platelets into the sinusoids. A greater number of sinusoidal capillaries and adipocytes can be seen in the specimen. In the bone marrow, all cells from the immune system are formed, except mature T cells. Therefore the bone marrow is a primary lymphoid organ.
The specimen shows the thymus, thymus (HE). In the preparation, the thymic lobes can be seen separated by dense connective tissue. At low magnification one can see that each lobe consists of a peripheral darker part (the cortex), and a central lighter part (the medulla). Both areas contain a dense stroma of epithelial reticular cells. These cells are stellate in shape and have light, oval nuclei. The majority of cells are immature T cells, or thymocytes. These are significantly more numerous in the cortex, which is why it stains more darkly. In the medulla we find red-stained Hassall corpuscles of flattened reticular epithelial cells filled with keratohyaline granules. The thymus is the only organ in the body that generates mature T cells. Therefore, the thymus is a primary lymphoid organ.
Secondary lymphoid organs
The specimen is a lymph node, nodus lymphaticus (HE). The lymph node is surrounded by a connective tissue capsule from which trabeculae extend inwards. The parenchyma is divided into a cortex and a medulla. The capsule is separated from the cortex by a lighter area of subcapsular sinuses. These are areas where lymph from afferent lymphatic vessels collects before it enters the lymph nodes. Afferent lymphatic vessels are usually lost during isolation of the organ. The subcapsular sinuses continue into the intermediate sinuses, which follow the course of the trabeculae consisting of dense connective tissue and drain into the medulla. The cortex consists of two parts: the outer and inner cortex. The outer cortex contains B cells, whereas the inner cortex contains B cells. Only the B cells can form secondary lympoid follicles, visible as ball-like structures with a lighter and a darker area, which are temporary structures in which B cells of high antigen affinity are selected. Both the inner and outer cortex contain a network of reticular cells and fibers. The medulla is made up of medullary strands of lymphatic tissue and medullary sinuses, both of which contain many lymphocytes, plasma cells and myeloid cells. Lymph is finally collected in the hilus, which drains into the efferent lymphatic vessel.
The specimen is a lymph node, nodus lymphaticus (HE).
The specimen is the spleen, lien (HE). The spleen is covered by a thick outer capsule of dense connective tissue. A number of trabeculae, also consisting of dense connective tissue, enter the parenchyma or pulp of the spleen from capsule. The parenchyma consists of a red and white pulp. The white pulp consists of a central artery with a sheath of lymphatic tissue (periarterial lymphatic sheath, PALS). The inner sheath consists of T cells, whereas the outer sheath is made up of B cells. Surrounding the PALS is a thin margnial zone containing large blood vessels, or sinuses, from which specialized antigen-presenting cells capture blood-borne antigens. If there is a secondary lymph node within the white pulp. Between the white pulp we can find the red pulp, consisting of Billroth's tracks. The red pulp also contain numerous venous sinuses, which are involved in the capture and elimination of old (effete) red blood cells. In this specimen, the red pulp is much more pronounced than the white pulp.
The specimen is the spleen, lien (HE). This slide clearly shows the cords of Billroth in the red pulp.
The specimen is a palatine tonsil, tonsilla platina (HE). At the surface of the specimen, towards the lumen, a multilayered squamous epithelium is visible, which invaginates into the lamina propria, forming crypts. The lamina propria is almost completely made up of lymphocytes. Whereas they can be segregated into B and T cell zones using immuno-histochemistry, they do not form an inner and outer cortex as in the lymph node. Various secondary lymph nodes can be seen in the B cell zones. At the bottom of the crypts, lymphocytes can be found to infiltrate the the epithelium.The lower part of the tonsil is defined by a thick capsule of dense irregular connective tissue, which reaches all around the tonsil up to the squamous stratified epithelium of the oral cavity.
Tonsil II - Longitudinal section
This slide also shows the lingual tonsils (HE). However, this slide is cut longitudinally, which shows the crypts as cavities in the middle of the tissue. We can also see some skeletal muscle tissue and a mucous salivary gland in this specimen.
The specimen is a cross-section of the appendix, appendix vermiformis (HE). This structure is part of the colon, but is considered an immunological organ. It has a narrow and irregular lumen. The mucosa is made up of simple columnar epithelium that invaginates into the lamina propria, forming simple tubular glands, or crypts oif Lieberkühn, which are highly numerous in the rest of the large intestine. The lamina propria is filled with a large amount of lymphocytes that extend into the submucosa. The submucosa, tella submucosa, is made up of well-developed connective tissue. The tunica muscularis, the muscle layer, is made up of bundles of smooth muscle fibers in two layers (inner circular and outer longitudinal). The surface of the appendix is made up by a tunica serosa.
The digestive system
The oral cavity
The specimen is the lip, labium (HE). The outer surface of the lip is covered with stratified squamous keratinized epithelium, or thin skin. There are also longitudinally cut hairs, pili, which grow from follicles in the dermis. Attached to the hear sheath, we can see several small sebaceous glands, gll. sebaceae, which release sebum in this canal. The inner surface of the lip is covered with stratified squamous pseudo-keratinized or non-keratinized epithelium. Mucous glands, gll. labiales, are located in the connective tissue of the lamina propria. The border between the keratinized and non-keratinized epithelium is a sharp line on the red edge of the lip. In this place, the connective tissue papillae are extremely deep, and the blood vessels are located close to the surface of the epithelium, giving the lips their characteristic red color.
The specimen is the lip, labium (HE). This preparation is darker in color then Lip-I, which allows for better observation of the musculature.
The specimen is the upper surface of the tongue, dorsum linguae (HE). It is covered with squamous, keratinized epithelium lying on a lamina propria. The protrusions of the lamina propria are the lingual papillae - papillae linguales. The tongue contains four types of papillae (i.e. Filiform, fungiform, foliate and vallate). This specimen shows densely arranged filamentous papillae - papillae filiformes, which are heavily keratinized, especially at their tips. During preparation of the specimen, much of the dead keratinized layer is lost, which is why we see it only at the tips of the papillae as bright pink coverings. The papillae filiform provide a rough surface that facilitates
movement of food during chewing. For this reason, the epithlium and underlying lamina propria are heavily folded in ridges and papillae to provide stronger adhesion between the layers. Beneath the mucosa, mostly in the submucosa, we find both serous and mucous glands. Underneath, we observe a very thick layer bundles of skeletal muscle arranged in multiple directions, which allows extensive manipulation of food entering the oral cavity.
The specimen is the upper surface of the tongue, dorsum linguae (HE). It shows the dorsal end of the tongue, where we find much fewer filliform papillae and instead, we observe pseudostratified epithelium. This speciment shows the 'walled' papilla - papilla vallata. The papilla is surrounded by a fold, or wall, which gives the papilla its name. This wall raises the papilla above the level of the surrounding mucous membrane and is covered with pseudostratified squamous epithelium. Between the papilla and its wall is a depression, or trench. In this trench, the serous von Ebner glands open, which start in the connective tissue directly under the papilla and reach deep between the bundles of muscle cells. In the epithelium of the trench, on the side of the papilla, we can see the taste buds - caliculi gustatorii. The taste buds are made up of spindle-shaped sensory and supporting cells arranged like "barrels" with a depression in the middle into which the cilia of the sensory cells protrude.
Teeth
The specimen is dental pulp, pulpa dentis (HE), which is the inner tissue mass insode of a tooth. Under low magnification, unformed loose connective tissue with numerous arterioles and blood capillaries, some of which are filled with blood, are visible. Under high magnification, the nuclei of endothelial cells protruding into the lumen are visible in the walls of the blood capillaries.
The preparation is part of the tooth crown (ground tissue). The base of the tooth crown is made up of dentin, substantia eburnea covered by enamel, substantia adamantina. Due to the method of preparation, only the inorganic part of the tissue is visible in the specimen. In the dentin area, longitudinally arranged dentinal tubules can be seen, which are covered by darker enamel. Within the dentin, areas of interglobular dentin are visible - areas in the preparation that are darker due to the smaller amount of minerals that remain between the calcospherite spheres during dentin mineralization (shaped like a lowercase letter m). At the dentin-enamel border, enamel defects are visible at high magnification: enamel bushes, spindles and lamellae. Enamel is made up of enamel prisms that gently curve and extend from the enamel-dentin junction to the free enamel surface. Obliquely arranged Retzius stripes are visible in the enamel (corresponding to the increase in mineralization during enamel growth and development). By examining the preparation under a microscope without light (one can do this by covering the light source on the microscope with your hand), it is possible to see white-silver areas in the enamel: Hunter-Schreger stripes, which occur as an optical phenomenon due to the different refraction of light passing through differently placed enamel prisms.
The specimen is a part of the tooth root (ground tissue). The base of the tooth root is made up of dentin, substantia eburnea covered with cementum. Due to the method of preparation, only the inorganic part of the tissue is visible. The specimen shows longitudinally arranged dentinal tubules covered with cellular cementum. At the border of dentin and cementum is Toms' granular layer - a darker colored granular area of irregularly mineralized dentin. Peripherally, we see a homogeneous layer which is made up of hyaline dentin. Cementum continues to this layer and contains cementocyte lacunae. The tubules that emerge from the lacunae, which in vivo contain cementocyte outgrowths, are oriented towards the outer surface of the tooth. Between the lacunae in the cementum, parallel-laid tubules are visible, which are filled with Sharpey's periodontal fibers during life.
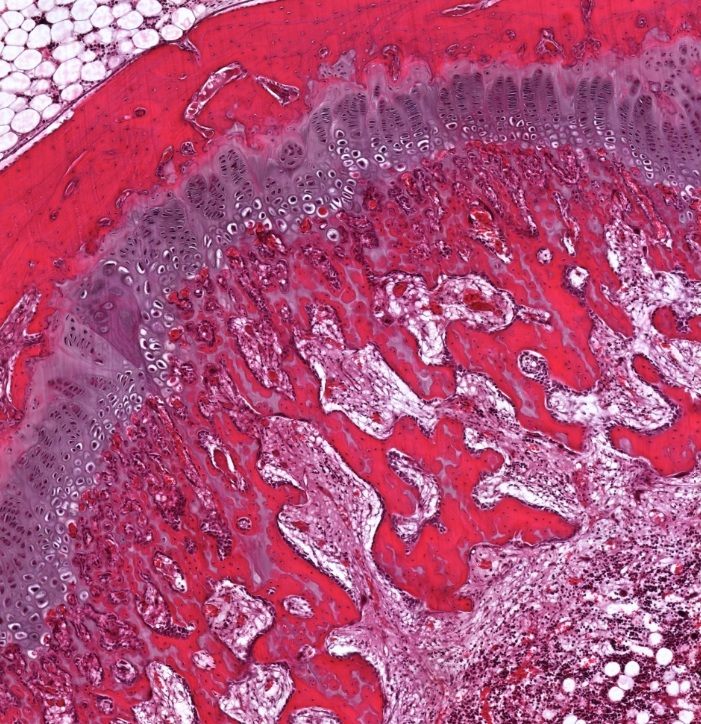
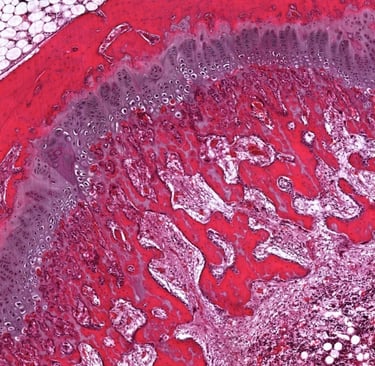
Gingiva I
The specimen is a tooth in the dental alveolus (decalcification + HE). Next to the part of the tooth crown (which lacks enamel due to the decalcification process during preparation) the oral mucosa protrudes from the dental alveolus and forms the gums, or gingiva. The gingiva are made up of 1. the multilayered squamous epithelium of the oral cavity that has a thin layer of keratin on its surface, 2. the connective tissue of the lamina propria with deep connective tissue papillae, and 3. thick collagen fibers that attach the mucosa to the alveolar bone and to the tooth (periodontal ligaments). The part of the gingiva that adheres to the tooth enamel forms the gingival pocket and is made up of a thin multilayered squamous epithelium without connective tissue papillae. This tissue has a cuticle on the free surface that is structured like a basal lamina - Gottlieb's epithelial junction, with which it is firmly attached to the tooth.
The specimen is a tooth in the dental alveolus (decalcification + HE).
The specimen is a tooth in the dental alveolus (decalcification + HE). The specimen shows a tooth attached to the jawbone by periodontal ligaments. The bundles are formed by collagen fibers. Note that the ligaments pull the tooth upward, thereby reducing the pressure of the tooth on the bone during chewing.
The specimen is a tooth in the dental alveolus (decalcification + HE).
The specimen is a tooth in the dental alveolus (decalcification + HE).
The specimen is a tooth in the dental alveolus (decalcification + HE).
The gastroinstestinal tract
The specimen is a cross-section of the first 1/3 of the oesophagus, esophagus (HE). The slide shows that the wall of the esophagus is made up of the following layers (from the luman outwards): 1. mucosa (tunica mucosa); this layer can be subdivided in a. the lamina epithelialis (in the submucose maden up of a multilayered squamous non-keratinized epithelium), b. the lamina propria (loose connective tissue) and c. lamina muscularis mucosae (bundles of smooth muscle fibers); 2. submucosa (tella submucosa): loose connective tissue Here we also find clusters of seromucous glands, gll. oesophageae; 3. muscularis externa (tunica muscularis) made up of bundles of skeletal muscle cells that form an inner circular and outer longitudinal layer separated by connective tissue; 4. outer layer (tunica adventitia) of light connective tissue. Note that in the middle of the oesophagus, the muscularis externa transits from skeletal to smooth muscle. The lower 1/3 of the oesophagus ois therefore exclusively made up of smooth muscle.
The specimen is a part of the wall of the body of the stomach, corpus ventriculi (HE). We can see that the gastric mucosa is covered by a single-layered cylindrical epithelium that folds deep into the lamina propria, forming gastric pits. Several branched tubular gastric glands, gll. gastricae propriae, open into each of these pits, which fill the entire width of the lamina propria. The reticular connective tissue that makes up the lamina propria is therefore only visible as thin lines underneath the epithelial folds. The glands extend to the lamina muscularis mucosae, which can be seen as a layer of smooth muscle of 5-10 cells thick directly underneath the gastric pits. Below the muscularis mucosae is a thin layer of submucosa (tella submucosa) made of loose connective tissue. Next follow three layers of the muscularis externa (tunica muscularis) made of bundles of smooth muscle cells separated by connective tissue. At high magnification, the individual types of cells that make up the gastric glands can be seen: Facing the lumen and reaching down into the pits until the neck region we find mucous cells that produce an alkaloid mucuous that protects the inner cell wall of the stomach from gastric juices. In the neck region and at the upper part of the glands we find parietal cells, large round cells with and of eosinophilic cytoplasm and a round, centrally located nucleus, which produce hydrochloric acid and intrinsic factor. In the basal part of the glands we find some lining cells, and chief or zymogenic cells of basophilic cytoplasm with secretory granules. In the basal area there are also enteroendocrine cells that cannot be distinguished using a regular HE staining.
Small intestine I - longitudinal section
The specimen is a cross-section of the wall of the small intestine, intestinum tenue (HE), in the jejunum. On the slide, it is possible to see Kerckring's circular folds of the submucosa, the plicae circulares, which can also be seen macroscopically. At higher magnification, we can see that the mucosa of the small intestine folds outwards in branches called intestinal villi, or villi intestinales. Intestinal villi are built by the epithelium and the lamina propria. The lamina muscularis mucosae does not participate in the structure of the villi, but can be seen in the plicae circulares. Villi are covered with a single layer of cylindrical epithelium. The epithelial cells in this layer, the enterocytes, have a finger-like extensions of their cytoplasma called microvilli into the lumen, which greatly increases the contact surface with the contents of the lumen. Mucous-filled goblet cells, single exocrine cells, are located between the enterocytes and can be seen as lighter-stained bubbles in the epithelial lining. Simple tubular glands called Lieberkühn's crypts, can be found at the basis of the villi and extend through the entire thickness of the lamina propria to the lamina muscularis mucosae. Enterocytes in the glands do not have microvilli yet. At the bottom of these glands are Paneth cells with large eosinophilic granules filled with antimicrobial peptides called defensins. Here, we also find stem cells, which differentiate into enterocytes, paneth cells or goblet cells. Underneath the plicae circulares we see the well-vascularised submucosa. Underneath that, we find two layers of smooth muscle, the tunica muscularis esterna. The outer surface of the small intestine is made up of the tunica serosa, a layer of connective tissue on which we find mesothelium, a single-layered squamous epithelium.
Small intestine II - cross section
This slide shows a transverse section of the small intestine, specifically the jejunum. Note the extreme flexure of the tissue that maximizes the contact surface area.
The specimen is a cross-section through the wall of the large intestine, intestinum crassum or colon (HE). The lamina propria of the colon is filled with a large number of simple tubular glands - Lieberkühn's crypts (on longitudinal and transverse sections) that extend to the laminae muscularis mucosae. The surface of these glands is made up of a single layer of cylindrical epithelium, containing colonocytes, which resemble the enterocytes from the small intestine, but have much fewer microvilli. Between the colonocytes, in the eithelium, we find a large number of goblet cells, which are much more frequent in number than in the small intestine, thus giving the glands a flower-like appearance. The lamina propria also contains many lymphocytes. Surrounding the epithelium and lamina propria we find a thin layer of the muscularis mucosa, made up of smooth muscle cells. The submucosa is made up of dense connective tissue and contains many individual lymphocytes as well as some larger nodes of lymphocytes which form lymph node-like structures, which in the ilium are called Peyer's patches. Peripherally from the submucosa is the muscularis externa, made up of bundles of smooth muscle cells. Three longitudinally oriented bundles pf muscle cells that only cover part of the outer layer called taenia coli are also part of the colon, but cannot be seen on this specimen. The outer layer of the colon is made up of a serosa or adventitia, dependent on the part of the colon.
Organs associated with the digestive system
The salivary glands
The specimen is a parotid gland, gl. parotid (HE). At low magnification, the lobes of the salivary gland can be seen, separated by connective tissue within which are larger blood vessels, nerves and interlobular drainage ducts lined with double-layered cubic epithelium. The parenchyma of the gland is made up of serous acini with a very narrow lumen, lined with pyramidal epithelial cells. The cells have eosinophilic cytoplasm and large, round nuclei. Around the terminal parts of the acini are basket-shaped myoepithelial cells with thin, flattened nuclei. Between the terminal parts of the glands are intralobular drainage ducts - striated ducts or secretory tubes lined with single-layered cubic epithelium with a pale eosinophilic cytoplasm. Adipocytes can also found within the parenchyma. The parotid gland differs from the other salivary glands in that it is exclusively serous, with no mucous glands.
The submandibular salivary gland
The specimen is a submandibular salivary gland, gl. submandibularis (HE). At low magnification, the salivary gland lobes can be seen separated by connective tissue, within which are located larger blood vessels, nerves and interlobular drainage ducts lined with double-row cuboidal epithelium. The parenchyma of the gland is mixed, even though it is made up mostly of serous acini with somewhat fewer tubule-shaped mucous tglands. Serous acini with a very narrow lumen are lined with pyramidal epithelial cells. The cells have an eosinophilic cytoplasm and large, round nuclei. Mucous tubules are lined with cuboidal cells, basally located nuclei and a pale basophilic cytoplasm. On the peripheral parts of some mucous tubules there are Gianuzzi's crescents, also called demilune, which are clusters of serous cells. Around the terminal parts of the gland there are basket-shaped myoepithelial cells with thin, flattened nuclei. Between the terminal parts of the glands are intralobular drainage ducts - striated ducts or secretory tubes. Adipocytes are also found within the parenchyma.
The pancreas
The specimen is the pancreas, pancreas (HE). At low magnification, the lobes of the gland can be seen separated by connective tissue, inside which are larger blood vessels and interlobular drainage ducts lined with double-layered cubic epithelium. The parenchyma of the gland is made up of serous terminal parts with a very narrow lumen, lined with pyramidal epithelial cells. The cells have a two-tone cytoplasm (darker at the base, lighter at the apex) due to the presence of zymogenic granules, and a large, round nucleus. In the center of the acinus are centroacinar cells. The pancreas does not contain striated ducts as found in the salivary glands. Between the terminal parts of the glands are intralobular drainage ducts lined with single-layered cubic epithelium. Within the parenchyma are the endocrine parts of the pancreas - the islets of Langerhans, built of small polyhedral endocrine cells and fenestrated blood capillaries. They can be distinguished as small spots of a few hundred cells with a slightly paler staining than the surrounding exocrine pancreas.
The liver
The specimen shows the liver, hepar (HE). The functional unit of the liver is the liver lobule, a polygonal structure made up mostly of hepatocytes and sinusoid capillaries, around a central vein (v. centralis). In humans, the lobules are not sharply delimited because there is little interlobular connective tissue. At the point where three or more lobes meet, there are interlobular or Kiernan's portal spaces, also called the portal triad. These contain three types of canals: 1. venes, arteries and bile ducts, along with connective tissue. The vein has a wide lumen filled with erythrocytes, the artery has a much smaller lumen and thick walls, whereas the bile duct is lined with a single-layer cubic epithelium. The lobule is made up of hepatocytes arranged in plates that flow radially towards the center where the v. centralis is located. Between the hepatocytes are sinusoids that guide mixed arterial blood and venous blood derived from the vena porta towards the v. centralis.
The specimen is a liver, hepar (Mallory trichrome) of a pig. Structurally, the swine liver is similar to the human liver. However, in the swine thin sheets of connective tissue mark the borders of the liver lobules. For educational purposes we therefore include this specimen to clearly understand the structure of the liver lobules.
The respiratory system
The nasal cavity
The specimen is a longitudinal section through the respiratory part of the nose, regio respiratoria nasi (HE). Several nasal turbinates are visible. The surface of the nasal turbinates is covered with respiratory epithelium; a pseudostratified columnar epithelium with the nuclei of cells arranged in 2-3 rows. At their apical side, these cells are ciliated, which can be seen at high maghnification. Between the columnar epithelial cells we can find goblet cells (unicellular endo-epithelial glands), visible as lightly stained ovals in the epithelial layer. The epithelium also contains brush cells, small granule cells and basal cells, but these cannot be distinguished by HE staining. At high magnification, a thick basement membrane can be seen that separates the epithelium from the connective tissue on which it lies. Beneath the epithelium, in the connective tissue of the lamina propria, there are accumulations of lymphatic cells, as well as mixed seromucous gland (gll. nasales). Also, the nasal lamina propria contains a large networks of veins, the spongy body of the nose, allowing regulation of the hydration of the nasal secrete. The lamina propria continues into the perichondrium on those parts of the nasal septum and turbinates whose base is made of hyaline cartilage, or into the periosteum on parts whose base is made of bone tissue. This specimen does not contain cartilage.
Nasal cavity II - Murine (olfactory region)
The slide shows a section through the head of a mouse (H). The anatomy of a mouse is quite different from that of a human. However, this slide shows the curvature of the nasal cavity, which increases the contact surface between air and the respiratory epithelium. Its purpose is to warm and humidify the air before it enters the lower respiratory tract. Above the nasal cavity (left of the slide) we see the ethmoid bone through which bipolar neurons pass to the olfactory bulb. This area of the brain, which is much larger in mice than in humans (relatively), processes input from olfactory cells. The region of the nasal cavity that we see here is therefore the olfactory region. Its epithelium is made up of bipolar neurons, with cilia at the apical side, which contain the receptors for smell. In addition, we find columnar support cells and basal, stem cell-like cells.
The trachea
Trachea - I (Transversal section)
The specimen is a cross-section of the trachea (HE). The inner surface of the trachea is covered with a mucosa. Its top layer consists of respiratory epithelium, a cell layer consisting of pseudostratified cylindrical cells with cilia and goblet cells. The epithelium also contains brush cells, small granule cells and basal cells, but these cannot be distinguished by HE staining. The epithelium rests on a lamina propria in which there are mixed seromucous glands, gll. tracheales. The mucosa continues into a fibromuscular layer consisting of horseshoe-shaped, hyaline cartilage covered with a perichondrium. Facing the oesophagud is no cartilage, but can we see bundles of smooth muscle cells (m. transversus tracheae). The outer surface of the trachea is covered with a layer of loose connective tissue - tunica adventitia.
Trachea - II (Longitudinal section)
The specimen is a longitudinal section of the trachea (HE). This slide shows cross-section of several cartilaginous rings lining the trachea, separated by elastic fibrous tissue.
The lungs
The specimen is taken from the lung, pulmo (HE). In the lung parenchyma, lobes are separated by connective tissue. Within the lobes, we find cross-sectioned bronchi, bronchioles and alveoli. The bronchus is a tube with a stellate-shaped lumen lined with respiratory epithelium (pseudostratified cylindrical epithelium with cilia and goblet cells), lying on a lamina propria. Bronchi also contain glands, gll. bronchiales, which can be mucous, serous and mixed. The mucosa also contains well-developed elastic fibers. Next, we find a fibromuscular layer containing plates of hyaline cartilage and spirally arranged smooth muscle fibers. The bronchi also often contain lymphocytes. The outer layer of the bronchi is made up of the tunica adventitia, which connects it with the surrounding tissue. This specimen contains two bronchi at the left most side of the specimen. The bronchiolus is a tube thinner than 1 mm in diameter, covered with a single-layer cylindrical or cubic epithelium without goblet cells. The connective tissue of the lamina propria, rich in elastic fibers, continues into a layer of circular smooth muscle cells. On the outside, the bronchiole is covered with the loose connective tissue of the tunica adventitia. Bronchioli do not contain cartilage or glands. Alveoli, alveoli pulmonis are air-filled sacs, lined with a single-layer of squamous epithelium, called pneumocytes type I. In some places inside the alveoli, cuboidal cells, called pneumocytes type II can be seen, which produce surfatant. Between the alveoli there is a dense network of blood capillaries with a small amount of connective tissue rich in elastic fibers and macrophages.
Skin and its derivates
Skin
The specimen is skin, integumentum commune (HE). This specimen was taken from the sole of the foot and shows thick skin. The surface of the skin is covered by a stratified squamous epithelium called epidermis. It is made up of five layers: 1. a single layer of cylindrical cells along the basal lamina, the stratum basale. Proliferation takes place in this layer and it also contains the melanocytes which give pigment to the skin. 2. several layers of cuboidal cells called the stratum spinosum. 3. a layer of cuboidal to squamous cells with clearly visible keratohyaline granules, stratum granulosum. 4. an eosinophilic, homogeneous layer which no longer shows nucei and is typically lighter in color than the surrounding tissues, stratum lucidum. And 5. a thick layer of keratinized tissue made up of dead squamous cells called stratum corneum. The boundary between the epithelium and the connective tissue on which it lies is irregular due to the connective tissue papillae that are imprinted into the epithelium. Beneath the epithelium is the connective tissue of the skin, dermis or corium, which is made up of a network of collagen, reticulin and elastic fibers, with a larger amount of ground substance. The part of the dermis that makes up the connective tissue papillae is loose connective tissue rich in blood vessels and is called the stratum papillare or papillary dermis. The deeper layer is made up of dense irregular connective tissue called the stratum reticulare or reticular dermis. Beneath the dermis is the hypodermis or subcutaneous connective tissue rich in fat cells.
The preparation is skin, integumentum commune (HE). This specimen shows thin skin. Thin skin has the same structure as thick skin. However, it is characterized by a much thinner stratum corneum and lacks a stratum lucidum. The epidermis rests on the papillary dermis, which tends to be less convoluted than in thick skin as it is sibject to less abrasion. Beneath the dermis is the hypodermis. At the border of the dermis and hypodermis, and in the hypodermis, are numerous sweat glands, gll. sudoriferae. Sweat glands are simple convoluted tubular glands that secrete according to the merocrine type. The surface of the skin is covered by a multilayered squamous epithelium - epidermis. I Their terminal parts on the cross-section have a circular shape, a visible lumen, and are lined with a single-layer epithelium made of pyramidal-shaped cells. The drainage ducts, which are darker on the preparations, are lined with a double-row cubic epithelium. Sebaceous glands, gll. sebaceae, are holocrine in the type of secretion. They are located next to the hair follicles. Their terminal parts have a sac-like appearance, without a lumen that is filled with secretion and dead cells. This type of gland is holocrine; their terminal parts are lined with several layers of epithelial cells in different stages of decay. In addition, we find several hair follicles. These are locted in the lower part of the dermis and reach all the way up to the epidermis. They are connected with a bundle of smooth muscle cells, the musculus erector pili, which can make the hair stand up.
This slide shows a thin section of skin where dye was applied to the dermis while the tissue was still alive, commonly known as a tattoo. The dye is absorbed by skin macrophages, which generally retain it for life. In this slide, the dye therefore marks the skin macrophages as dark red.
This slide shows a section of thin skin isolated from the axillary region, which is a pyramid-shaped anatomical space located below the shoulder joint (also called arm pit). This site shows the three types of glands found in the skin. The first are the sebaceous glands, holocrine glands that usually deposit their secretions in the hair shaft, as can be seen here. The second type is the eccrine sweat glands. These glands can be found on most parts of the skin and have an unusual type of stratified cuboidal epithelium. The basal layer contains pale-stained transparent cells that produce most of the fluids in sweat. The lumen is lined with dark cells that contain granules with antimicrobial proteins. Surrounding the glands are myoepithelial cells. The third type of gland is the apocrine sweat gland, which can be found mainly in the apocrine and perineal regions. Apocrine glands have much larger lumens than eccrine glands and are composed of simple cuboidal cells with numerous secretory granules that mediate merocrine secretion. Their secretions are often metabolized by bacteria, which causes a characteristic odor.
Mammary glands
Mammary gland inactive phase - deep tissue
The specimen is a breast, mamma (HE) of an adult woman. The mammary gland is in the inactive phase. The specimen shows lobules made of connective tissue with a large amount of fat cells separated by dense connective tissue. The specimen shows glandular lobules consisting of intralobular ducts surrounded by loose connective tissue and dense interlobular connective tissue with occasional drainage ducts. The lactiferous ducts are lined with double-layered cubic epithelium.No secretory cells can be distinguished.
Mammary gland inactive phase - nipple
The preparation is the breast, mamma (HE) of an adult woman. The mammary gland is in the inactive phase. This specimen was isolated from the tissue directly below the nipple. At this site, the milk ducts, usually about 15-25 per mammary gland, converge to form the openings from which milk is produced during lactation. This site also contains much dense connective tissue that can be seen between the ducts.
Mammary gland - active phase (lactation)
The preparation is a breast, mamma (HE) in the active phase (lactation). The specimen shows glandular lobules made of connective tissue with a large number of alveoli in which the secretion is located. The alveoli are lined with a single-layer epithelium of varying height, which depends on the phase of secretion. The method of secretion of the breast is apocrine. The lobules are separated by dense connective tissue in which there are drainage channels, ductuli lactiferi, lined with double-layered cuboidal epithelium.
The urinary system
The urinary system
The preparation is a kidney, ren (HE). The kidney is made up of a darker stained cortex and a lighter stained medulla. In the cortex, we can find the renal corpuscle made up of glomeruli (a cluster of fenestrated blood capillaries) surrounded by the visceral and parietal sheets of the Bowman's capsule. The visceral sheet consists of highly specialized podocytes, whereas the parietal sheet is simple squamous epithelium. The space between is the intercapsular space and can be seen in the preparation as empty crescents surrounding the glomeruli. Between the renal corpuscles, we can see the differently sectioned proximal and distal tubules. The more numerous proximal convoluted tubules have epithelial cells of a pyramidal shape which have a distinctly eosinophilic cytoplasm, almost completely closing the lumen of the tubules. On the apical surface, they have a brush-like coating (microvilli). Their lateral borders are difficult to distinguish due to numerous intercellular interdigitations. The cells of the distal convoluted tubules are lower, of cuboidal shape and their lumen is wider than in the proximal tubules. Their cytoplasm is pale, and the lateral boundaries between adjacent cells are easily visible. The renal medulla consists of the the descending and ascending limbs of the loops of Henle, the collecting ducts and blood vessels (vasa recta). The thin segments of the loops of Henle are lined with a single-layered squamous epithelium, and can be distinguished from capillaries by the appearance of the cell and the shape of the nucleus.
The specimen is the ureter, ureter (HE). The ureter has a mucosa with transitional epithelium, a lamina propria, muscularis externa and tunica adventitia. The muscularis externa is made up of spiral bundles of smooth muscle.
The specimen is the urinary bladder, vesica urinaria (HE). The inner surface of the bladder wall is covered with a mucosa made up of transitional epithelium, a lamina propria of loose connective tissue without connective tissue papillae. The mucosa also contains a very thin, discontinuous lamina muscularis mucosae made up of smooth muscle cells. The muscularis externa in the bladder is made up of differently oriented bundles of smooth muscle cells, without strictly separated layers. The lateral and inferior sides of the bladder are covered by a tunica adventitia, whereas the top is covered by a serosa. This specimen is taken from an empty, relaxed bladder, where we can see the transitional epithelium as multiple layers of cuboidal cells. Note the umbrella cells facing the lumen, which are covering the rest of the epithelium.
The slide is of the urinary bladder, vesica urinaria (HE). The transitional epithelium of the urinary tract is unique in that it can transition between two forms. When empty, the epithelium is a pseudostratified cuboidal epithelium that appears as five to ten layers. When full, the epithelium expands and assumes a squamous form of only two or three layers. In this slide, we see the squamous form, while the previous slide shows a cuboidal form. It should be noted that in both states the lumen is surrounded by squamous roof cells that protect the underlying tissue from damage by urine.
The endocrine system
The endocrine system
The specimen is the pituitary gland, gl. pituitaria (HE). at its outer surface, the pituitary gland has a capsule of connective tissue. The parenchyma can be divided in two parts. The darker part on the right is the adenohypophysis, made up of strands and clusters of endocrine cells and is interspaced with many fenestrated blood capillaries. The endocrine cells have different affinities for histological dyes and are therefore histologically divided into basophilic or eosinophilic cells.The adenohypophysis also contains chromophobice cells, which are palely stained cells that typically do not produce hormones and include stem cell like-cells. The light-stained left part of the specimen is the neurohypophysis, which is mostly made up of the unmyelinated axons of neurons which have their cell bodies in the hypothalamus. In addition, we find pituicytes, which are astrocyte-like glial cells, and numerous fenestrated capillaries. On this specimen we see how the neurohypothysis extends into the infundibulum, which is the stalk-like region that connects it with the hypothalamus. This region is surrounded by the pars tuberalis of the adenohypophysis. Hormones derived from the infundibulum enter the blood stream of the adenohypohysis here and stimulate release of other hormones by this part of the organ. The adenohypohysis is further divided in the pards distalis, which makes up most of the organ and the pars intermedia, in between the neuro- and adenohypohysis. Here we typically find Rathke's cysts, which are remnants of the embryonic Rathke's pouch from which the adenohypohysis is formed.
The specimen is the pineal gland, corpus pineale or epiphysis cerebri (HE). It consists of lobes of pinealocytes, which are irregular-shaped neuro-endocrine cells that produce the hormone melatonin. In addition, we fins some nerve fibers from diencephalon-derived neurons and glial cells. Thin connective tissue septa invade the gland and connect to the pia mater which covers its surface. Red-stained calcifications - brain sand or acervulus cerebri - can be seen in the pineal gland.
The specimen is a thyroid gland, gl. thyroidea (HE). It consists of a large number of irregular follicles between which we find sparse connective tissue with many blood capillaries. The follicular cells lining the follicles can be low cylindrical, cubic or squamous, depending on their functional state. Inside the follicles there is a red-stained colloid, mostly consisting of the horomone precursors thyroglobulin. This is converted into thyroxine and tri-iodothyronine upon stimulation by the pituitary gland. Parafollicular or C cells, which produce calcitonine, are located next to the follicles (within the basal lamina) or form special clusters between them, but are much less numerous than follicular cells. Parafollicular cells are typically 2-3 times larger than follicular cells and have a pale cytoplasm.
The specimen is an adrenal gland, gl. suprarenalis (HE). Surrounding the gland is a capsule of dense irregular connective tissue. The parenchyma of the gland is divided into a cortex and a medulla. The cortex of the adrenal gland has three zones: the zona glomerulosa, which makes mineralocorticoids, is made up of round clusters of glandular cells and is located directly under the connective tissue. The zona fasciculata, which makes glucocorticoids, is the thickest zone in which the cells form columns that run parallel and perpendicular to the surface of the gland. Between the columns of cells there are fenestrated blood capillaries. In the cytoplasm of the cells of the zona fasciculata there are a large number of small fat droplets that dissolve during the preparation of the slide. These cells, also called spongiocytes or foam cells, therefore appear full of small vacuoles. The zona reticularis, which produces weak androgens, is located at the border with the medulla and is made up of small cells that form irregular network. The adrenal medulla is made up of polygonal cells that form bands surrounded by reticulin fibers and an abundant network of blood capillaries. It produces epinephrin and norepinephrin (adrenalin and noradrenalin).
The male reproductive system
The male reproductive system
The specimen shows the, testis and epididymis (HE). In the parenchyma of the testis we find convolutedly coiled seminiferous tubules. Inside the tubules there are spermatogenic cells in different stages of development, which are completelz engulfed bz large, supporting Sertoli cells. The tubules are surrounded by lamellar connective tissue. Between the tubules there are interstitial Leydig cells with large nuclei and red cytoplasm. The testis is surrounded by a red-colored, thick sheath of dense connective tissue called the tunica albuginea. In the part of the tunica albuginea facing the epididymis, the connective tissue is interrupted by fissured spaces lined with a single-layered cubic to squamous epithelium called the rete testis. Tubules with a scaloped epithelium, called the ducti efferentes connect the testis to the epididymus. They have an irregular lumen, as they are lined with clusters of cubic cells with cilia (kinocilia) that alternate with those without cilia, giving them a wavy surface. The epididymis itself is a single tube with a regular round or oval lumen, and is lined with two layers of cells: cubic cells along the basal lamina and cylindrical cells on the surface. The surface cells at the apical pole have large branched microvilli - stereocilia. The tubules are surrounded by connective tissue rich in smooth muscle cells. The preparation also shows the efferent ducts of the head of the spermatic cord, which have been cut multiple times.
The specimen is a transverse section of the spermatic cord, funiculus spermaticus (HE). Several structures can be seen within the spermatic cord. The largest structure is the transverse section of the vas deferens, ductus deferens. It has a narrow lumen covered by a stratified columnar epithelium with stereocilia, a thin lamina propria rich in elastic fibers, and is surrounded by a thick lining of smooth muscle cells arranged in three layers. Next to the vas deferens in the cord is the cremaster muscle, a muscle made of transversely striated skeletal muscle. Furthermore, we can find the many veins of the pampiniform plexus, multiple arteries, and the nerves innervating the testis.
The specimen is a prostate gland (HE). The parenchyma of the gland is made up of tuboalveolar glandular parts covered with cubic or multi-row cylindrical epithelium surrounded by abundant fibromuscular stroma. Some glandular parts contain bright red round prostatic stones called prostatoliths, which we find in the lumen of the glands. The prostate can be segregated in a central zone with sub mucosal glands, a transitional zone with mucosal glands and a peripheral zone with the main glands. Two transversely cut drainage ducts are also visible in the specimen.
The female reproductive system
The female reproductive system
The specimen is an ovary, ovarij (HE). The ovary is surrounded by a single layer of squamous to cuboidal cells called the germinal epithelium. Underneath we find the tunica albuginea, a thin layer of dense irregular connective tissue. The ovarian parenchyma consists of a cortex and a medulla. The cortex of the ovary (zona parenchymatosa) is made of connective tissue with numerous follicles in various stages of development or regression. The primordial follicles are seen most superficially. These are small and consist of a primary oocyte and a single layer of flattened follicular cells. Primary follicles can be single-layered - when the primary oocyte is surrounded by a single layer of follicular cells or multilayered - when the primary oocyte is surrounded by several layers of cells. Secondary (vesicular) follicles contain a cavity (antrum foliculli) filled with fluid (liquor foliculli). Granulosa cells that surround the oocyte and protrude into the lumen of the cavity of the secondary follicle form the cumulus oophorus. The mature follicle is also called the antral or Graffian follicle. It contains an oocyte surrounded by granulosa cells, which typically form a stalk that connecs it to the granulosa cells that line the lumen. Surrounding these cells we find the theca interna and theca externa, which are important for the production of estrogen. The ovarian medulla, rich in numerous blood and lymphatic vessels located in connective tissue, is also called the zona vasculosa. In this specimen we also see the ampulla of the oviduct, which has a highly convoluted internal surface.
The specimen is a cross-section through the ampullary part of the fallopian tube, ampulla tubae uterinae (HE). Numerous folds of the mucosa covered by a single-layered cylindrical epithelium with a well-vascularized lamina propria are visible. Some epithelial cells have cilia while others secrete nutrients for the zygote. The muscularis externa is made up of bundles of smooth muscle fibers. On the outer surface we find a serosa, connective tissue covered by a serous membrane.
Uterus I - Proliferative phase
This specimen shows the uterus, uterus (HE) in the late proliferative phase of the uterine cycle. The lining of the uterus, the endometrium, is covered with a simple cylindrical epithelium that in some places invaginates into the lamina propria forming glands, gll. uterine. Some cells of the superficial epithelium have cilia. The lamina propria contains a large number of stromal cells (fibroblasts) and abundant ground substance. The superficial, thicker layer of the endometrium is called the zona functionalis. Numerous uterine glands are visible in the deeper layers of the lamina propria. The darker-stained part of the endometrium that is located immediately next to the myometrium, is called the zona basalis. From this layer the superficial part of the endometrium is regenerated after menstrual bleeding or after childbirth. Beneath the endometrium is the myometrium, a thick layer of muscle tissue made of bundles of smooth muscle cells separated by connective tissue.
This specimen is the uterus, uterus (HE) in the early secretory phase of the uterine cycle. The endometrium is covered with a simple cylindrical epithelium that invaginates into the lamina propria forming glands, gll. uterine. The glands are convulated and deposite their secretion into the lumen of the uterus. The lamina propria contains a large number of stromal cells (fibroblasts), abundant ground substance and numerous blood vessels. The superficial layer of the endometrium or zona functionalis in this phase of the cycle has two parts: the superficial layer or stratum compactum with a greater number of cells and the deeper layer or stratum spongiosum which has a greater amount of ground substance. The darker-stained part of the endometrium that is located immediately next to the myometrium, is called the zona basalis. From this layer the superficial part of the endometrium is regenerated after menstrual bleeding or after childbirth. Beneath the endometrium is the myometrium, a thick layer of muscle tissue made of bundles of smooth muscle cells separated by connective tissue.
This specimen is the birth channel, vagina (HE). The vagina is covered by a stratified squamous non-keratinized epithelium. Underneath, we find a relatively thin lamina propria, rich in elastic fibers and with occasional accumulations of lymphocytes and neutrophils. The muscularis externa is made up of bundles of smooth muscle cells. We can see that the muscularis externa is very rich in blood vessels.
Organs of special sense
The Ear
The specimen is an outer ear, auricula (HE). At the base of the ear is an elongated plate of elastic cartilage surrounded by loose connective tissue called the perichondrium. At the surface of the outer ear we can find skin with numerous hairs with sebaceous glands. The connective tissue also contains sweat glands. In the hypodermis we can also find ample adipose tissue.
The specimen is an ear, auricula (orcein). At the base of the ear there is an elongated plate of elastic cartilage surrounded by loose connective tissue of the perichondrium. At higher magnification, a network of brown-colored elastic fibers in the intercellular matrix can be seen between individual clusters of chondrocytes called isogenic groups.
This specimen shows the internal ear (HE). We can see a cross-section of the cochlea and part of the vestibule. Its outer layer is formed by the bony labyrinth, labyrinthus osseus, which contains the membranous labyrinth, labyrinthus membranaceus, segregated by a thin liquid phase filled with perilypmh. In the cochlea, the bony labyrinth winds around the modiolus, which contains ganglions organized in spirals. A bony ridge, the lamina spiralis ossea, protrudes laterally and from here the basilar membrane originates. The space below it is the scala tympani, which is filled with perilypmh. Above it we can see the cochlear duct filled with endolymph. The triangular-shaped cochlear canal is separated by the vestibular membrane from the scala vestibuli. This channel also contains perilymph and is connected with the scala tympani at the top of the cochlea through a channel called the helicotrema. The perilymphatic space of the scale vestibuli and scala tympani are covered by a simple mesothelium. The wall of the cochlear duct facing away from the modiolus contains the stria vascularis, a special type of vascularized epithelium that secretes the endolymph of the entire inner ear. On the basilar membrane of the cochlear duct we can find the organ of Corti, a highly differentiated organ specialized in the detection of sound. It contains sensory and supporting cells that are covered by the tectorial membrane.
The eye
The specimen shows the eye, oculus (HE). In this specimen we will concentrate on the frontal segment. The cornea is the transparent anterior part of the outer eye membrane. It is made up of 5 layers: 1. a stratified squamous epithelium (5-6 layers of cells) whose surface cells have microvilli; 2. The Bowman's membrane, a homogeneous layer without cells made of collagen fibers and a thickened ground substance; 3. a thick stroma made up of dense regular connective tissue. It contains a large number of lamellae of collagen fibers that intersect at right angles, with some fibroblasts and amorphous ground substance; 4. The Descemet's membrane, a homogeneous mass with some collagen fibers; 5. A simple endothelium of the anterior chamber, of mesenchymal origin, typically squamous or cuboidal in shape. The ciliary body, corpus ciliare, is part of the middle eye. It is made up of the orbiculus ciliaris - a smooth part that begins at the serrated line, ori serrati and extends forward, and the ciliary processes, processus ciliares, which form the corona ciliaris. The base of the ciliary body is the ciliary muscle, which is triangular in shape in a cross-section. It is surrounded by a loose connective tissue with many elastic fibers, melanocytes and blood vessels. The surface of the ciliary body facing the vitreous, lens and posterior chamber is covered by the blind part of the retina. In this part, the retina is made up of two layers of epithelial cells: the outer, pigmented, stratum pigmenti corporis ciliaris and the inner, unpigmented, pars ciliaris retinae. The latter part participates in the secretion of aqueous humor. These two epithelial layers touch with their apical surfaces, which are interconnected by desmosomes. The fibers that connect the ciliary processes to the equator of the lens, the fiber zonulares, are continues with the basal lamina of the inner layer. The iris is a part of the middle layer of the eye that forms the aperture in the frontal plane in front of the lens of the eye with the pupil in the middle. The frontal surface is a discontinuous and uneven layer of fibroblasts and melanocytes, under which we find the connective stroma. The first layer is a connective tissue with few blood vessels and fibers, but rich in cells. This is followed by a well-circulated loose connective tissue in which the muscularis sphincter pupillae is located at the pupillary edge of the iris. The muscularis dilator pupillae is located along the entire length of the back side of the iris. Together, these muscle regulate the aperture of the pupil. The color of the iris depends on the amount of melanocytes in the stroma. The posterior surface of the iris is covered by the blind part of the retina. In this part, the retina is made up of two layers of epithelial cells, both pigmented: the outer, stratum pigmenti iridis, and the inner, pars iridica retinae. These two epithelial layers touch each other with their apical surfaces, which are connected to each other by desmosomes. The lens, lens cristalina, is a biconvex formation that is covered only at the front surface by a single-layer of cubic epithelium and is completely surrounded by a capsule. The base of the lens is made up of lens fibers. Regeneration of the lens occurs from the epithelium on the lateral side, which is why we can still find nuclei of cells in the lens parenchyma at the poles.
The specimen shows the eye, oculus (HE). In this specimen we will concentrate on the posterior segment, which contains the part of the retina specialized in the detection of light. The outer surface of the posterior eye contains the sclera, the opaque part of the outer eye, which is made up of dense connective tissue rich in collagen fibers with few cells. Therefore, this tissue normally has a white color. Beneath is the suprachoroidea lamina, made up of loose connective tissue rich in melanocytes that separates it from the middle eye membrane - the choroid. The choroid is made up of a layer of loose connective tissue rich in blood vessels, elastic fibers, melanocytes and numerous other cells. A thin homogeneous layer of Bruch's membrane separates it from the visual part of the inner eye membrane, the retina. The visual part of the retina, pars optica retinae, is made up of an outer pigment layer - stratum pigmenti retinae, and 9 inner layers as follows: 1. rod and cone layer, 2. outer limiting membrane, 3. outer granular layer, 4. outer reticular layer, 5. inner granular layer, 6. inner reticular layer, 7. optic nerve cell or ganglionic layer, 8. optic nerve fiber layer, 9. inner limiting membrane. There are also blood vessels between the cells and fibers of the inner 5 layers. The retina also contain Muller cells, which span from the nerve fiber till the rod and cone layer. The yellow spot, or macula lutea, rich in rods and the blind spot, where the optic nerve leaves the retina and leads to the brain, are not visible on this specimen.
Follow
+385 51 651 176
Contact
Faculty of Medicine
Department of histology & Embryology
Braće Branchetta 20
51000, Rijeka, Croatia